There is a link between MTHFR polymorphisms and schizophrenia. How do these gene variations impact the risk of MTHFR and schizophrenia? This article examines the connections, underlying mechanisms, and treatment implications.
Key Takeaways
MTHFR gene polymorphisms, particularly C677T and A1298C, are associated with reduced enzyme activity that influences folate metabolism, impacting health and predisposing individuals to conditions such as schizophrenia.
The MTHFR C677T polymorphism has been linked to an increased risk of developing schizophrenia, with ethnic differences influencing the degree of this genetic association and symptom severity.
Elevated homocysteine levels resulting from MTHFR polymorphisms are correlated with cognitive dysfunction in schizophrenia, indicating the critical role of biochemical imbalances in mental health management.
Understanding MTHFR Gene Polymorphisms
The MTHFR gene, located at 1p36.3 on chromosome 1, consists of 11 exons and is pivotal in maintaining intracellular folate levels by facilitating the conversion of certain forms of folate. This gene’s function is crucial for numerous biological processes, including DNA synthesis and repair, which underscores its importance in overall health.
Two common polymorphisms within the MTHFR gene, C677T and A1298C, have been identified as significant common mthfr gene variant that affect enzyme activity. These polymorphisms, including methylenetetrahydrofolate reductase gene polymorphisms, are known as gene variants that lead to varying levels of enzyme efficiency, which in turn can influence bodily functions that rely on folate metabolism.
Individuals with the methylenetetrahydrofolate reductase mthfr C677T TT genotype experience significantly reduced enzyme activity, sometimes below 30% of normal levels. This reduction can have profound effects on the body’s ability to process folate, which is essential for numerous cellular functions. Similarly, the A1298C polymorphism results in decreased enzyme activity, contributing to various health issues.
Understanding these MTHFR gene variants is crucial because they represent common genetic vulnerabilities that can predispose individuals to health conditions, including mental disorders. The interplay between these polymorphisms and folate metabolism highlights the importance of genetic factors in health and disease.
Exploring the mechanics of the MTHFR gene and its polymorphisms sets the stage for understanding their broader implications, particularly in the context of schizophrenia. This foundational knowledge allows for a deeper understanding of how these genetic variations influence mental health outcomes.
MTHFR C677T Polymorphism and Schizophrenia Risk
The MTHFR C677T polymorphism has been increasingly recognized as a significant factor in schizophrenia risk. This polymorphism affects the folate metabolic pathway, which is crucial for brain function and mental health. The presence of the T allele in this gene variant is statistically associated with an increased risk of developing schizophrenia, highlighting its role as a candidate genetic risk factor.
Patients with the TT genotype of the MTHFR C677T polymorphism exhibit a notable increase in schizophrenia risk compared to those with the CC genotype. This genetic variation can significantly impact folate metabolism, leading to biochemical changes that predispose individuals to psychiatric conditions.
Research has shown that ethnic differences play a role in how MTHFR variants influence psychiatric conditions. For instance, certain populations may demonstrate a stronger correlation between MTHFR variants and schizophrenia, suggesting that allele frequencies and genetic backgrounds can affect the manifestation of mental disorders.
The link between the MTHFR C677T polymorphism and schizophrenia risk underscores the importance of genetic polymorphisms in mental health. It also raises questions about how these genetic variations interact with other factors, such as environment and lifestyle, to influence the onset and progression of schizophrenia.
Moving forward, it’s important to explore how folate metabolism, influenced by MTHFR polymorphisms, plays a crucial role in mental health. This will further illuminate the complex interactions between genetics and psychiatric disorders.
The Role of Folate Metabolism in Mental Health
Folate metabolism, orchestrated by the MTHFR gene, is essential for brain function and mental health. The MTHFR gene’s role in processing one-carbon metabolism affects both folate and homocysteine levels, which are critical for neurogenesis and cognitive function.
Variants in the MTHFR gene, particularly C677T and A1298C, are linked to reduced enzyme activity, which may lead to various psychiatric disorders. These genetic variations can result in abnormalities in one-carbon metabolism, negatively impacting brain regions such as the cortex and hippocampus, which are vital for cognitive and emotional processes.
Folate deficiency, combined with the MTHFR C677T polymorphism, can exacerbate symptoms in schizophrenia. Research indicates that while overall folate supplementation may not significantly improve negative symptoms for all schizophrenia patients, it potentially benefits those with specific MTHFR genotypes. This suggests a personalized approach to dietary interventions could be more effective.
Dietary folate intake significantly influences enzyme activity in individuals with MTHFR gene variants, impacting mental health outcomes. Studies have shown that dietary folate can mitigate the effects of MTHFR genetic polymorphisms on schizophrenia, highlighting the importance of nutrition in managing mental health.
Understanding the role of folate metabolism in mental health provides a crucial link between genetic variations and psychiatric disorders. It emphasizes the need for personalized nutritional strategies to manage and potentially alleviate symptoms of schizophrenia and other mental disorders.
DNA Methylation and Schizophrenia
Epigenetic modifications, such as DNA methylation, play a significant role in the development of schizophrenia. These modifications are influenced by folate levels, which are in turn affected by MTHFR polymorphisms. Aberrant DNA methylation patterns mediate the association between MTHFR polymorphisms and the severity of schizophrenia symptoms.
Patients with MTHFR polymorphisms tend to exhibit more severe schizophrenia symptoms, suggesting a direct link between genetic variations and symptom severity. In early-onset schizophrenia, a distinct hypomethylated pattern is observed, differing significantly from the methylation levels found in adult-onset cases.
Differentially methylated positions in early-onset schizophrenia patients show significant hypermethylation and hypomethylation across relevant genes. These epigenetic changes can affect gene expression, potentially leading to the development and progression of psychiatric disorders.
Moreover, the mean global methylation levels in patients with schizophrenia are lower compared to healthy subjects, particularly in those with the TT genotype. This underscores the role of MTHFR polymorphisms in influencing genomic dna methylation and highlights the potential for targeted interventions to address these changes.
Understanding the interplay between DNA methylation and schizophrenia provides a deeper insight into how genetic and epigenetic factors contribute to mental health disorders. This knowledge is crucial for developing more effective and personalized treatment strategies.
Clinical Phenotypes and Genetic Variation in Schizophrenia
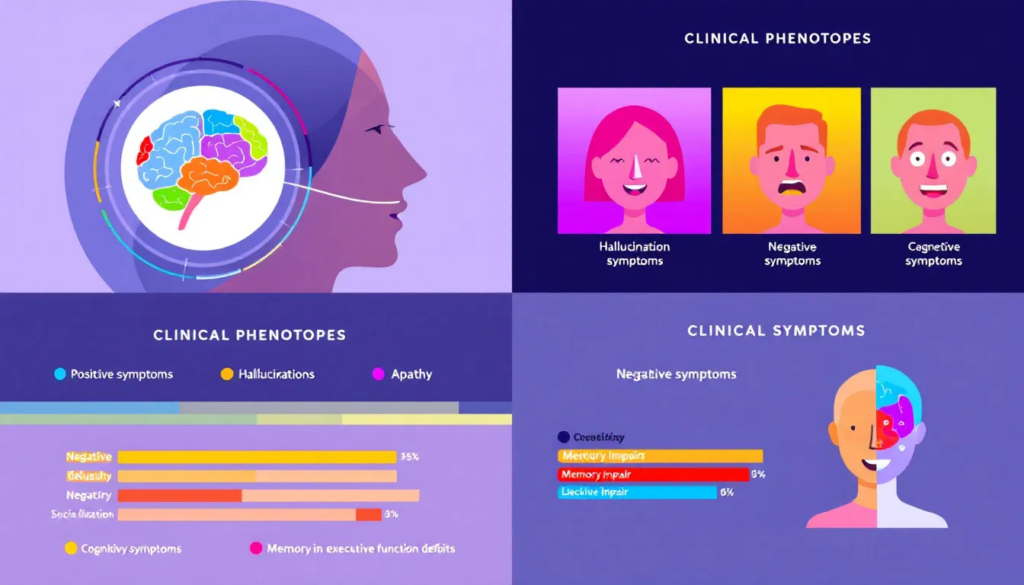
Clinical phenotypes of schizophrenia can vary widely among patients, and genetic variations in the MTHFR gene play a significant role in these significant differences. Differences in allele frequencies of the MTHFR C677T polymorphism can help differentiate between schizophrenia and bipolar disorder patients, highlighting the genetic impact on psychiatric disorders.
The T allele is associated with an earlier onset of bipolar disorder symptoms, indicating that genetic variations can influence the age of onset for psychiatric conditions. Conversely, the C allele is more common in healthy controls than in patients with schizophrenia and bipolar disorders, suggesting a protective effect against these mental disorders.
A subgroup analysis revealed that the link between the MTHFR C677T polymorphism and schizophrenia is particularly strong in Asian populations, emphasizing the role of ethnic differences and the significant difference in genetic susceptibility. This highlights the importance of considering demographic factors in genetic association studies.
Genetic variations in the MTHFR gene can influence cognitive functions and symptom severity in schizophrenia patients. For instance, a correlation exists between PANSS scores and MTHFR polymorphisms in early-onset schizophrenia patients, indicating the severity of symptoms is linked to these genetic variations.
Patients with early-onset schizophrenia tend to exhibit more severe symptoms than those with adult-onset schizophrenia, emphasizing the influence of MTHFR variations. The higher prevalence of MTHFR polymorphisms in early-onset schizophrenia patients suggests a distinct clinical phenotype associated with these genetic factors.
Homocysteine Levels and Cognitive Function in Schizophrenia
MTHFR gene polymorphisms can lead to elevated levels of homocysteine, a condition linked to several health issues, including cognitive dysfunction. Elevated homocysteine levels are frequently detected in schizophrenia patients, suggesting a biochemical link between MTHFR polymorphisms and mental health.
High homocysteine levels can lead to neuronal apoptosis, which negatively impacts cognitive function in schizophrenia patients. This is particularly concerning as it affects executive function and information processing speed, crucial aspects of cognitive performance.
Cognitive dysfunctions in schizophrenia are influenced by genetic variations in the MTHFR gene, with higher homocysteine levels correlating with the severity of negative symptoms. Moreover, homocysteine is linked to oxidative stress, which can exacerbate schizophrenia symptoms.
Research indicates that metabolic syndrome in schizophrenia patients is associated with higher homocysteine levels, further complicating their health status. However, folic acid and vitamin B12 supplementation have shown promise in lowering homocysteine levels and improving symptoms in schizophrenia, offering a potential therapeutic approach.
Understanding the impact of homocysteine levels on cognitive function in schizophrenia highlights the importance of addressing biochemical imbalances in managing mental health disorders. This knowledge can inform more effective treatment strategies aimed at improving cognitive outcomes for patients (doi 10.1016).
Environmental Factors and Schizophrenia Onset
Environmental factors play a significant role in the onset and progression of schizophrenia, often interacting with genetic predispositions such as MTHFR polymorphisms. Research indicates that nutritional deficiencies during pregnancy, particularly folate deficiency, can significantly increase the risk factors for developing schizophrenia. This highlights the importance of maternal nutrition in the early stages of development.
Dietary folate intake directly influences the activity of the MTHFR enzyme, which can help mitigate some of the risks associated with its polymorphisms. Ensuring adequate folate levels through diet or supplementation can potentially offset the negative effects of MTHFR genetic variations on mental health.
The interaction between MTHFR polymorphisms and environmental factors like nutrition suggests a complex web of influences on schizophrenia risk. The presence of the T allele in MTHFR polymorphisms is associated with increased schizophrenia risk and may influence cognitive and behavioral outcomes. This underscores the need for comprehensive approaches that consider both genetic and environmental factors in managing mental health.
Evaluating how environmental factors interact with MTHFR polymorphisms is crucial for understanding mental health outcomes and developing effective prevention and intervention strategies. This holistic approach can help identify at-risk individuals and tailor interventions to their specific needs.
Potential Treatment Strategies
Potential treatment strategies for schizophrenia patients with MTHFR polymorphisms should focus on addressing the underlying biochemical imbalances. L-methylfolate supplementation is one promising approach, as it can enhance methylation processes and alleviate psychiatric symptoms in individuals with MTHFR mutations. This form of folate is readily utilized by the body, bypassing the need for conversion by the MTHFR enzyme.
Ketamine has also shown promise in treating treatment-resistant psychiatric disorders, including schizophrenia. Unlike traditional antidepressants, ketamine acts rapidly by blocking NMDA receptors, which enhances synaptic plasticity and neurotransmitter production. This rapid action can provide much-needed relief for patients who do not respond to conventional treatments.
The ability of ketamine to promote neuronal plasticity may help patients restructure harmful thought patterns and behaviors, offering a new avenue for managing schizophrenia symptoms. However, it is essential to work with a practitioner who understands genetics and the specific genes associated with schizophrenia, as well as the role of free copper and biotoxins in mental health.
By combining genetic insights with innovative treatment strategies, healthcare providers can develop more effective and personalized approaches to managing schizophrenia. This holistic approach can improve patient outcomes and enhance the quality of life for those affected by this challenging disorder.
Future Directions in Research
Future research should focus on further elucidating the relationship between MTHFR gene polymorphisms and schizophrenia. While significant progress has been made, there is still much to learn about how these genetic variations influence the development and progression of mental health disorders.
Longitudinal studies and intervention trials are necessary to clarify the long-term effects of MTHFR polymorphisms on schizophrenia risk and symptom severity. These studies can provide valuable insights into how genetic and environmental factors interact over time, informing more effective prevention and treatment strategies.
Additionally, more research is needed to explore the potential benefits of personalized medicine in psychiatric care. Tailoring interventions to an individual’s genetic makeup allows healthcare providers to develop more targeted and effective treatment plans, thereby improving patient outcomes.
The importance of understanding the interplay between genetics and environmental factors cannot be overstated. Future research should aim to uncover the mechanisms by which these factors influence mental health, paving the way for more comprehensive and effective approaches to managing schizophrenia and other psychiatric disorders.
Summary
Throughout this exploration, we have delved into the complex relationship between MTHFR gene polymorphisms and schizophrenia. From understanding the basic mechanics of the MTHFR gene to examining how its variations influence mental health, we have uncovered critical insights into the genetic and environmental factors that contribute to this challenging disorder.
As we look to the future, the importance of personalized medicine and innovative treatment strategies becomes increasingly clear. By combining genetic insights with a holistic approach to mental health care, we can develop more effective interventions, improving the lives of those affected by schizophrenia. The journey of understanding and addressing mental health challenges continues, promising a brighter future for patients and their families.
Frequently Asked Questions
What is the role of the MTHFR gene in mental health?
The MTHFR gene is vital for folate metabolism, impacting brain function and mental health. Variations in this gene can alter enzyme activity, affecting levels of folate and homocysteine, which may influence mental well-being.
How does the MTHFR C677T polymorphism increase schizophrenia risk?
The MTHFR C677T polymorphism, especially the TT genotype, significantly reduces enzyme activity and disrupts folate metabolism, contributing to biochemical changes that elevate the risk of schizophrenia.
Can dietary folate intake influence the effects of MTHFR polymorphisms?
Dietary folate intake can indeed influence the effects of MTHFR polymorphisms by enhancing the activity of the MTHFR enzyme. Adequate folate levels may help reduce the risks associated with these genetic variations.
What are the potential treatment strategies for schizophrenia patients with MTHFR polymorphisms?
L-methylfolate supplementation and ketamine therapy are effective treatment strategies for schizophrenia patients with MTHFR polymorphisms, as they target the biochemical imbalances associated with the condition. Implementing these approaches may lead to improved management of schizophrenia symptoms.
Why is further research needed on MTHFR polymorphisms and schizophrenia?
Further research on MTHFR polymorphisms and schizophrenia is essential to clarify their relationship and how genetic and environmental factors interact. Such studies could lead to improved prevention and treatment strategies for the condition.

